Preventive
Even if you don’t have any pressing dental concerns, it’s still important to visit the dentist for your biannual checkups. This gives us a chance to catch any issues
while they’re still small and provide you with a thorough, professional teeth cleaning to remove any built-up plaque before it causes cavities or gum disease.
Our preventive services include:
A dental sealant is a protective coating placed on the chewing surface of the back teeth to protect against cavities. Permanent back teeth have a significantly higher risk of developing decay as your toothbrush cannot reach the base of the grooves and pits on the biting surface of these teeth to clean them.

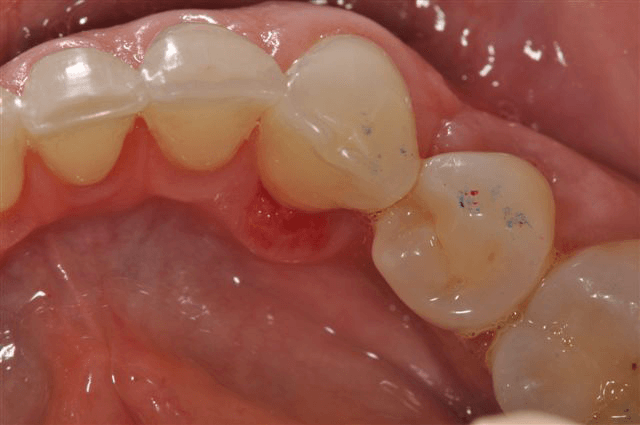
Before sealant placement

Preparing the teeth for sealants

After sealant placement
What are Dental Sealants?
Dental sealants are thin, hard plastic coatings placed in the pits and grooves of teeth. Usually, they are needed on the chewing surfaces of the back teeth, but other teeth may also develop pits that need to be protected with sealants.
Who should have Dental Sealants?
Dental sealants are most commonly placed on the permanent molars of children. Ideally, this is done shortly after these teeth fully erupt. The first permanent molars erupt around age six and the second permanent molars erupt around age twelve. Dental Sealants can also protect vulnerable pits or grooves on adults’ teeth.
How do Dental Sealants work?
The pits and grooves on the back teeth may be too narrow for a toothbrush bristle to reach the base of them. This allows plaque and bacteria to accumulate, which increases the risk of tooth decay. Dental sealants fill those pits and grooves, thus decreasing the risk of tooth decay by preventing the accumulation of plaque and
bacteria.
How are Dental Sealants placed?
Placing dental sealants requires no anesthetic or drilling. The teeth must be kept isolated during the procedure. The tooth surface is cleaned and prepared then the sealant material is spread into the pits and grooves. The material either sets by itself or is cured with a light. Your dental professional will check to ensure the sealant does not interfere with chewing.
What are the risks of Dental Sealants?
There is very little risk of having dental sealants placed. Rarely, a sealant will leak and decay will form beneath it. Regular examinations by your dentist allow sealants to be repaired or replaced as needed.
What are the risks of not having Dental Sealants placed?
Without dental sealants, the risk of tooth decay increases significantly in teeth with deep grooves and pits. Once a tooth is decayed, it requires a filling and often becomes weaker due to the loss of sound tooth structure.

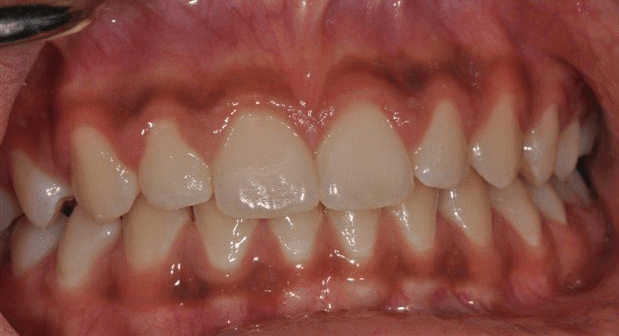
Before non-surgical periodontal therapy

After non-surgical periodontal therapy
What materials are used during Non-Surgical Periodontal Therapy?
The following materials and techniques may be used in your non- surgical periodontal therapy:
- Hand held instruments known as scalers and ultrasonics to clean the teeth.
- Local anesthetic (numbing) to control sensitivity.
- Antibacterial rinses to help decrease plaque and calculus.
- Antibiotic and antiviral pills to help kill bacteria and viruses and reduce the destructive response some people have to periodontal infections.
- Laser treatment to control bacterial levels around affected areas.
What are the benefits of Non-Surgical Periodontal Therapy?
Some potential benefits of non-surgical periodontal therapy include:
- Eliminating the infection present
- Controlling further infections and bone loss
- Reducing swollen and bleeding gums
- Reducing bad breath
- Avoiding tooth loss
- Decreasing the risk for diseases associated with periodontal disease such as cardiovascular disease, diabetes and rheumatoid arthritis
- Decreasing the risk of preterm low birth weight babies in pregnant women
What are the risks of Non-Surgical Periodontal Therapy?
Some potential risks following treatment may include:
- Tenderness of the gums for a period of time
- Open spaces developing between the teeth at the gum line due to shrinkage of previous swollen gums; these spaces may trap food and cause increased temperature sensitivity of the teeth for a period of time.
- Temporary tooth staining from certain antibacterial rinses
What are the alternatives to Non-Surgical Periodontal Therapy?
The alternatives to non-surgical periodontal therapy are:
- Surgical periodontal therapy
- No treatment
It is important to understand that periodontal disease is not curable. In the early stages, it may not even be noticeable to you. If you do not manage your disease by performing excellent home care, attending recommended cleaning intervals at your dental office, and adopting appropriate periodontal therapies, you must recognize the risk of further periodontal infection and ultimately tooth loss.
Periodontal disease is a term describing infection of the tissues which surround a tooth. There are two types of periodontal disease: ‘gingivitis’ is an infection and inflammation of the gums around the neck of a tooth whereas ‘periodontitis’ is an infection of the ligament and bone surrounding the root of a tooth.

Mild Periodontal Disease

Moderate Periodontal Disease

Severe Periodontal Disease
What causes Periodontal Disease?
Gingivitis occurs when plaque is allowed to build up around a tooth and create a sticky layer that causes gum infection. If you look in your mouth you will see redness, swelling, and bleeding of the gum around your tooth.
Periodontitis occurs in susceptible patients when a long-term gum infection is not treated. Infection and resultant inflammation lead to the loss of ligaments and bone around the root of your tooth. Factors which significantly increase the risk of developing periodontitis include:
- Genetics
- Smoking
- Diabetes
- Medications (certain anti-seizure, blood pressure, and immunosuppressant medications)
- Stress
- Poor Oral Hygiene
What can I do to minimize my risk of Periodontal Disease?
To minimize your risk of future periodontal disease, you must be mindful of the risk factors stated above. Gingivitis is usually well managed by adopting excellent oral hygiene practices. Periodontitis is more difficult to manage. Protocols recommended by your dentist may include:
Non-Surgical Periodontal Therapy
- Root cleaning (scaling and root planing) at the appropriate intervals to manage your risk for bone loss
- Antibacterial mouth rinses
- Oral antibiotics
- Customized home care instruction
- Smoking cessation counseling
- Surgical Periodontal Therapy
- Recontouring of gum and bone around affected teeth to allow better access for professional root cleaning and daily home care
Surgical Periodontal Therapy
- Recontouring of gum and bone around affected teeth to allow betteraccess for professional root cleaning and daily home care
How can an existing bite affect Periodontal Disease?
Bite problems on periodontally affected teeth can lead to accelerated periodontal disease and loosening of the teeth. If signs of a bite problem are present, the following may be considered to balance your bite and relieve excess pressure on periodontally involved teeth:
- Bite therapies including deprogramming and equilibration
- Orthodontic repositioning of the teeth
- Replacement of worn or damaged teeth
- Replacement of worn or damaged fillings
- Replacement of missing teeth
- Use of a custom-fitted bite guard to protect from grinding or clenching forces
What will happen if I choose to do nothing about my Periodontal Disease?
As uncontrolled periodontitis is progressive in nature, it will lead to increased bone loss and eventual tooth loss; ultimately affecting your ability to eat and speak. There are also connections between periodontal disease and other chronic diseases of the body such as cardiovascular disease, diabetes, and rheumatoid arthritis. In pregnant women, periodontal disease is strongly linked to preterm, low birth weight.

Worn teeth from grinding

Nightguard to protect teeth
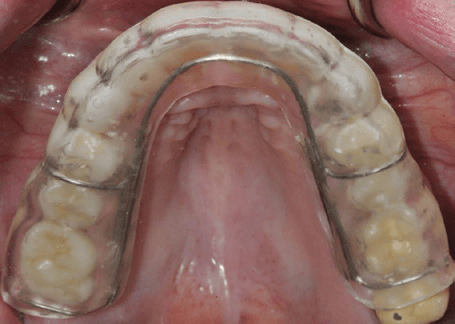
Nightguard to protect teeth
Why do I need a Nightguard?
Nightguards are needed to protect you from bite disorders, such as clenching and grinding, which may lead to abnormal tooth wear, muscle pain, and temporomandibular joint disorders [also known as TMJ disorders].
How is my Nightguard made?
Impressions are taken of your teeth and your night guard is custom made out of dental acrylic in a dental laboratory. On delivery of your nightguard, your dentist carefully adjusts and balances it to your support your bite, and jaw.
What is it like to wear my Nightguard?
Your nightguard may feel bulky or unusual at first. You may unconsciously take it out at night because of the unfamiliar feeling. Most people adapt to wearing a nightguard within a few weeks and often find they sleep better with the appliance than without it.
How long do I need to wear my Nightguard?
You should wear your nightguard every night, unless told otherwise by your dentist. Bringing your nightguard to your re-care appointments allows your dentist to examine it and assess its effectiveness.
How do I care for my Nightguard?
Clean your nightguard every time you clean your teeth. Gently brush your appliance with a small amount of toothpaste on your toothbrush and rinse with warm water. Any time the nightguard is out of your mouth, keep it safe in its retainer box. To help prevent staining, leave your nightguard in a 1:1 solution of white vinegar and water while it is out of your mouth.
What will happen if I choose not to wear my Nightguard?
If you choose not to wear your nightguard, your teeth will be at risk for continued night time wear.
Also, tooth sensitivity may increase, your jaw muscles may become progressively more sore and jaw joint problems may worsen over time.
Dental x-rays are valuable diagnostic tools that enable your dentist to search for hidden dental diseases such as cavities, gum and bone disease, abscesses, cysts, and tumors. X-rays are also used to view the progress of eruption of permanent teeth in children, for orthodontic and implant treatment planning, and many other dental procedures.
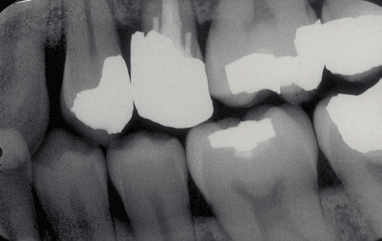
Bitewing X-Ray
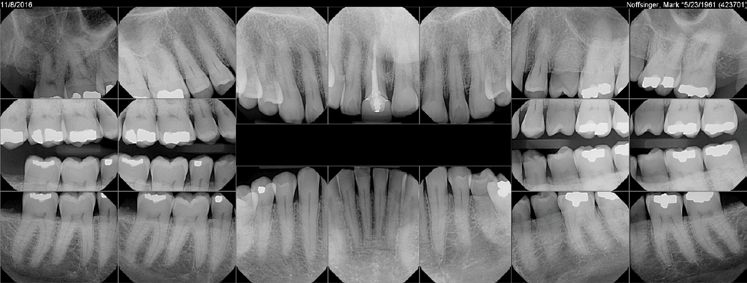
Full Mouth Series X-Rays
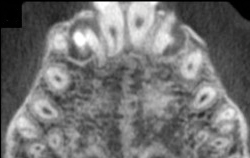
CBCT image
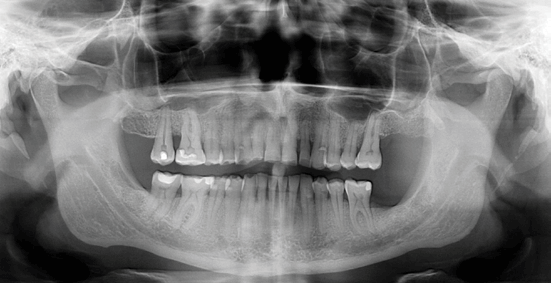
Panoramic X-Ray
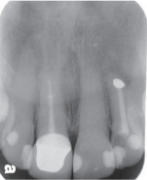
Periapical X-Ray
How often should I have Dental X-Rays taken?
The American Dental Association has guidelines for how often dental x-rays should be taken. The recommendations for each depend on their current dental and medical history as well as the condition of their mouth. Those with increased risk for dental problems may need x-rays as often as every six to twelve months, while others with no recent dental issues may require x-rays less often.
What are the types of Dental X-Rays I may have taken?
- Bitewings – A set of four x-rays that show the teeth above the gum line and the bone between the teeth. They allow your dentist to see bone loss and cavities between the teeth.
- Periapical – A single x-ray of a specific area including the tooth root and surrounding bone. These images help your dentist detect any unusual changes in the root and surrounding bone structures.
- Full mouth set – A combination of bitewing and periapical x-rays consisting of up to 20 films. This complete set of detailed x-rays helps your dentist diagnose cavities, abscesses, periodontal disease, impacted teeth, and other disease processes.
- Panoramic – A dental x-ray that captures the entire mouth in a single image, including the teeth, upper and lower jaws, surrounding structures, and tissues. This large image can show impacted teeth, cysts, Bitewing X-Ray Periapical X-Ray tumors, or other hidden structures, however, may not be helpful for early cavity detection.
- Cone Beam Computed Tomography or CBCT – One of the newest imaging technologies which capture three-dimensional pictures of soft tissue and bone. Your dentist may recommend a CBCT for various applications including dental implant planning, evaluation of the jaws and face, cleft palate assessment, endodontic (root canal) diagnosis or diagnosis of dental trauma.
How much radiation am I being exposed to with Dental X-Rays?
The amount of radiation from dental x-rays is negligible. Four bitewing x-rays have been estimated to be the amount of radiation received from a one to two-hour airplane flight.
Are there ways to limit radiation from my Dental X-Rays?
- Digital x-rays significantly reduce the level of radiation, by as much as Full Mouth Series X-Rays Panoramic X-Ray CBCT image 70-80%, utilizing sensors that replace traditional photographic x-ray film.
- Your dentist uses the “As Low As Reasonably Possible” (ALARA) method to customize x-ray frequency based on your risk factors to minimize your exposure.
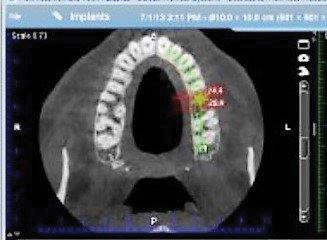



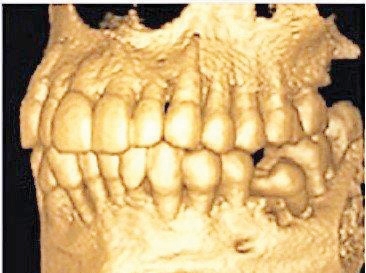
What are the benefits of a Dental CBCT scan?
The benefits of a Dental CBCT scan are that it:
- Provides 3-D images of dental structures, soft tissues, nerve paths and bone which are considerably more detailed than conventional two-dimensional dental x-rays.
- Allows for more precise diagnosis and treatment planning.
- Is simple and comfortable to take and can diagnostically image both bone and soft tissue simultaneously.
What are the common uses of a Dental CBCT scan?
Dental CBCT scans are commonly used to:
- Evaluate the position of teeth, bone structure, jaw joints and the airway.
- Aid in:
– Accurate placement of implants
– Surgical planning for the removal of impacted wisdom teeth
– 3-D orthodontic evaluation
– Complex root canal diagnosis and treatment
What are the risks of a Dental CBCT scan?
Although relatively low, Dental CBCT scans cause some radiation exposure; the amount of exposure is approximately the same as taking a five-hour international plane flight. Due to radiation exposure, scans are not generally recommended for pregnant women and should be used cautiously in the pre-orthodontic evaluation of children.
How does a Dental CBCT scanning procedure work?
During the scan, a motorized arm rotates 360-degrees around your head while capturing multiple images from different angles that are then reconstructed to create a single 3-D image.
Who interprets the results of a Dental CBCT scan?
The interpretation of a Dental CBCT scan may be done by your dentist, dental specialist, or radiologist.
Mouth Lesions: Colored Areas
Mouth Lesions (or colored areas) can be red/purple, brown, or black. They are more common in people over 60 and are typically located either under the tongue or at the back of the roof of the mouth.
Gum inflammation
Gum pigmentation
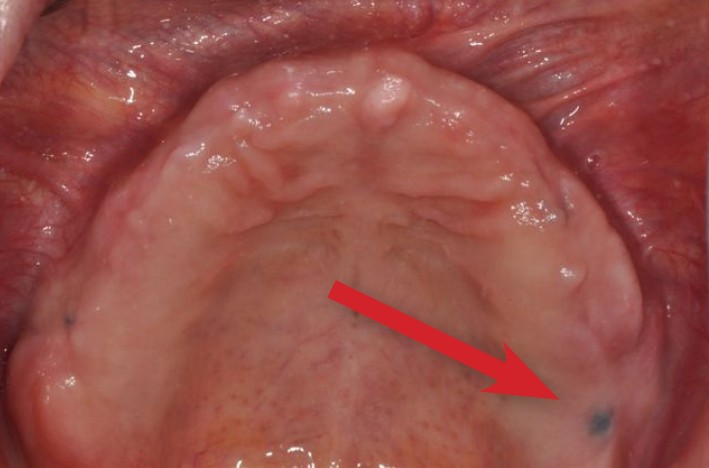
Amalgam Tattoo
What causes Colored Areas?
Red/Purple Areas are most often an indication of inflammation, infection, trauma, or surface blood vessels. Blood conditions such as thrombocytopenia and amyloidosis can create red/purple areas in your mouth. People who smoke, have dry mouth, or have a weakened immune system are more susceptible to yeast infections that cause inflammation and may appear as reddened areas with a white covering. Oral infections may be reddened and appear raised when compared to the surrounding tissue. People with bite problems, broken teeth, or an ill-fitting denture may have traumatized or inflamed tissues that look red and even ulcerated. Blood vessels tend to become more apparent in your mouth as you age and they show up as red/dark purple bumps.
Brown Areas are usually caused by pigmentation in the gums or lining of your mouth. Ethnic populations with darker skin tones tend to have these brown areas and are a variation of normal mouth tissue appearance.
Black Areas are usually benign “amalgam tattoos” and occur when gums or tissues are traumatized during the placement or removal of silver fillings. Amalgam tattoos do not grow or change over time and do not pose a health risk. However, black areas can indicate a more serious condition, so it is important to have your dentist determine what has caused this darker coloration.
What is my role in managing Colored Areas?
Note the size, location and duration of the area. Determine if it is painful and recall if you may have traumatized the area. If a colored area persists beyond one week, have it examined by your dentist.
What will happen if I do nothing about Colored Areas?
Although some colored areas are normal variations of mouth tissue, many indicate underlying disease processes. If your colored area is caused by inflammation or infection, it will likely get worse as time
goes on. If it is caused by ongoing trauma, it will also worsen with time. In the rare event that it is cancer, it can lead to disfigurement or death if not diagnosed and treated in a timely manner.
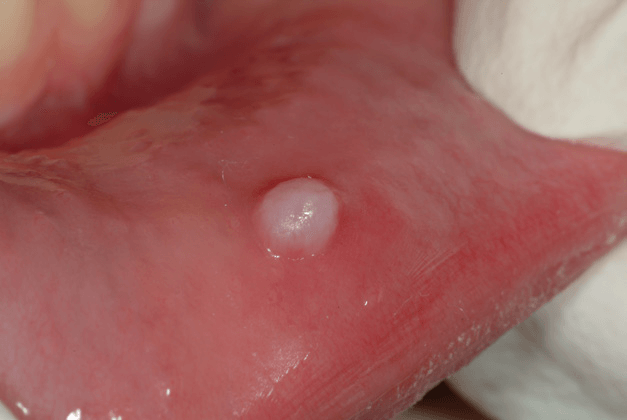
Mouth Lesions: Swelling
Swelling in your mouth can have several causes. These commonly range from infection, trauma and blocked salivary glands to normal bonegrowth. Less commonly, mouth swellings may be due to cysts or tumors.

Bony “Tori”

Dental Abscess
Tumor

Cyst
What causes Mouth Swellings?
Swellings in your mouth may be due to the following:
- Tooth or gum infections
- Trauma from bite problems or an ill fitting denture
- Blocked salivary glands
- Cysts
- Tumors
- Normal anatomy of your mouth (i.e., bony growths called “tori” that can develop over time near the base of your teeth)
Who is at high risk for Mouth Swellings?
People with untreated bite problems, heavily restored teeth, badly broken down teeth or advanced gum disease are at higher risk for dental infections and are therefore more likely to experience mouth
swellings. People with compromised immune systems are also at higher risk for developing mouth infections and therefore swelling.
People with an ill fitting denture may develop swelling where the denture rubs. People with untreated bite problems may also traumatize their cheeks and tongue resulting in swelling.
Less commonly, diseases such as Sjogren’s Syndrome or mumps may lead to swelling in the mouth.
What is my role in dealing with Mouth Swellings?
Pay attention to the size, shape, color, consistency, location, appearance and duration of the swelling. If the swelling lasts longer than one week, grows in size, becomes painful or recurs over time you must have the area examined by your dentist.
What can happen if I do nothing about the Mouth Swellings?
Ignoring swelling in your mouth can be dangerous. If the swelling is due to an infection it can cause serious damage to your body and may ultimately be life threatening. In the rare event that it is cancer, it can lead to disfigurement or death. Both of these types of swellings must be diagnosed and treated in a timely manner.
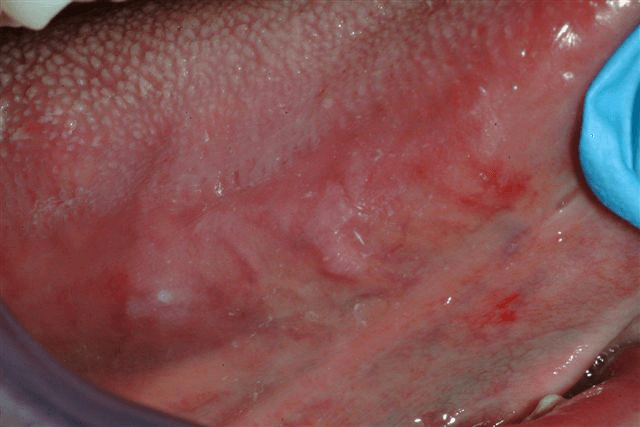
Mouth Lesions: Ulcer
Swelling in your mouth can have several causes. These commonly range from infection, trauma and blocked salivary glands to normal bonegrowth. Less commonly, mouth swellings may be due to cysts or tumors.
Canker Sore or “Aphthous Ulcer”

Red Ulcer (Erosive Lichen Planus)

Oral Cancer
What causes Mouth Ulcers?
Mouth ulcers may be caused by the following:
- Hot or spicy food
- Repeated rubbing from an ill fitting denture
- Stress (canker sores or “aphthous ulcers”)
- A viral infection
- Erosive Lichen Planus (an autoimmune disorder)
- Cancer
Who is at risk for Mouth Ulcers?
Most mouth ulcers are caused by trauma (pizza burns) or stress (canker sores). People with weakened immune systems may be more susceptible to both canker sores and certain viral infections which show up as groups of small ulcers in the mouth. Trauma from an ill fitting denture may also cause ulcers. More rarely, mouth ulcers may be caused by cancer.
What is my role in managing Mouth Ulcers?
Note the size, appearance, location and duration of the ulcer. Determine if it is painful, and recall if you may have traumatized the area. If an ulcer persists beyond one week, have the area examined by your dentist.
What can happen if I do nothing about my Mouth Ulcer?
If the ulcer is the result of a disease process, it may worsen if left untreated. If it is caused by ongoing trauma, it may also worsen with time. In the rare event that it is cancer, it can lead to disfigurement or death if not diagnosed and treated in a timely manner.
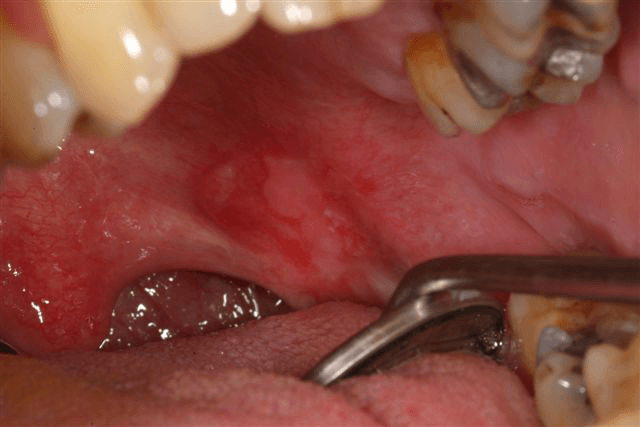
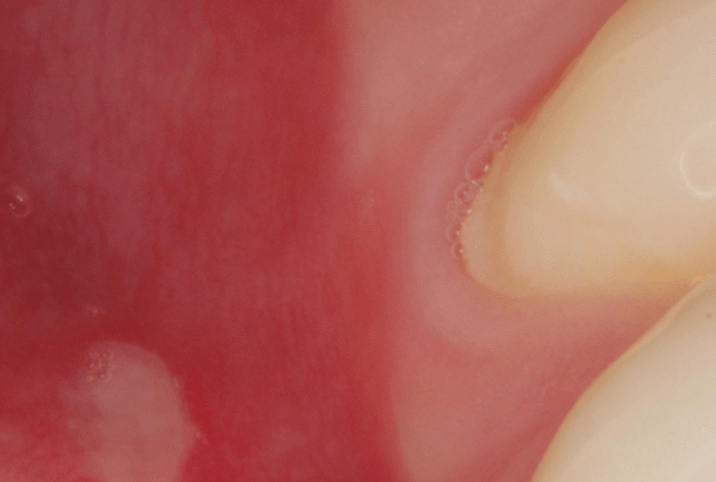
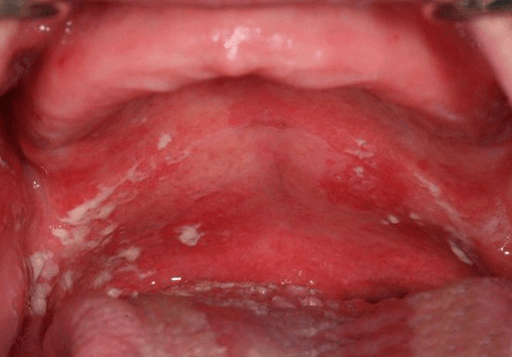
Mouth Lesions: White Spots
Most white spots are thickenings of normal mouth tissue in response to some form of irritant.
The white spot may be firmer than the surrounding tissue due to this thickening.
Less commonly, white spots can indicate an infection or disease process.
Oral Cancer on the side of the tongue
“Fibroma” from Cheek Biting

“Lichen Planus”
Yeast Infection on the roof of the mouth associated with an upper denture
What causes White Spots?
White spots in your mouth may be due to the following:
- Chronic cheek biting causing scar tissue or a “Fibroma” to form
- Smoking
- Repeated rubbing from an ill fitting denture
- Repeated rubbing from chewing food on gums in an area where teeth have been lost
- Yeast infection
- Lichen Planus (an autoimmune disorder)
- Syphilis
- Cancer
Who is at risk for White Spots?
People who smoke and those who experience dry mouth or a weakened immune system are more susceptible to yeast infections, which may appear as white spots. People who smoke often develop white areas in their mouth, which are caused by tissue irritation from the smoke. People who grind their teeth commonly develop
white lines on their cheeks from trauma. Trauma also causes areas of whiteness when a denture is ill fitting or food rubs against a ridge area where teeth have been removed.
What is my role in managing a White Spot?
Note the size, location, and duration of the spot. Determine if it is painful and recall if you may have traumatized the area. If a white spot persists beyond one week, have the area examined by your dentist.
What can happen if I do nothing about the White Spots?
If the white spot is the result of a disease process or a yeast infection, it will likely worsen if left untreated. If a white spot is caused by ongoing trauma, it will also worsen with time. In the rare event that it is cancer, it can lead to disfigurement or death if not diagnosed and treated in a timely manner.
Patient Feedback
EXCELLENTTrustindex verifies that the original source of the review is Google. Great staff and care at Bend Dental Wellness!Trustindex verifies that the original source of the review is Google. We have been going here for 5 years. We really enjoy how kind all of the staff are. Up to date modern tools.Trustindex verifies that the original source of the review is Google. I had an emergency and they found a way to get me in to be seen the same day. The staff and Dr Quigley were helpful and professional. I’ve been going to Bend Dental Wellness for four years and it has always been professional and friendly.Trustindex verifies that the original source of the review is Google. Dr. Blake Q and his staff are very friendly and competent. I did choose this practice because of his 'better' practices with dental care. And I've been very satisfied with my dental care for the past 3+years and will continue. Had a cleaning today with Mara and she was very gentle and thorough.Trustindex verifies that the original source of the review is Google. The service was excellent, both my teeth cleaning and discussion of possible future needs.
Request An Appointment
Need help? Contact us!