Restorative
If your teeth need some extra TLC, we’re here to help. We have a range of restorative treatments to restore your smile’s health, beauty, and functionality. Whether you have missing, damaged, painful, or decayed teeth, our skilled team can work with you to regain your oral health.
Our restorative services include:
Dr. Quigley utilizes the SMART amalgam removal technique as a framework for our amalgam removal protocols. The complete SMART amalgam removal protocols can be followed as outlined in the IAOMT’s guidelines, or we can customize the specific points to allow for individual preferences or tolerances. Since some of these recommendations can be difficult for patients due to the increased appointment length and use of additional barriers, Dr. Quigley will review these guidelines and customize them according to the patient’s preferences.
Utilizing the available scientific evidence, the IAOMT has developed extensive safety recommendations for removal of existing dental mercury amalgam fillings, including detailed protective measures that are to be utilized for the procedure. The IAOMT’s recommendations build upon traditional safe amalgam removal techniques such as the use of masks, water irrigation, and high volume suction by supplementing these conventional strategies with a number of additional protective measures, the need for which have only recently been identified in scientific research.
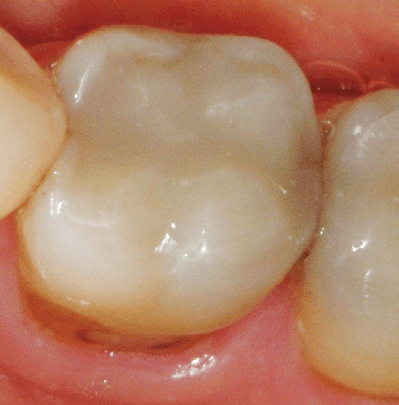
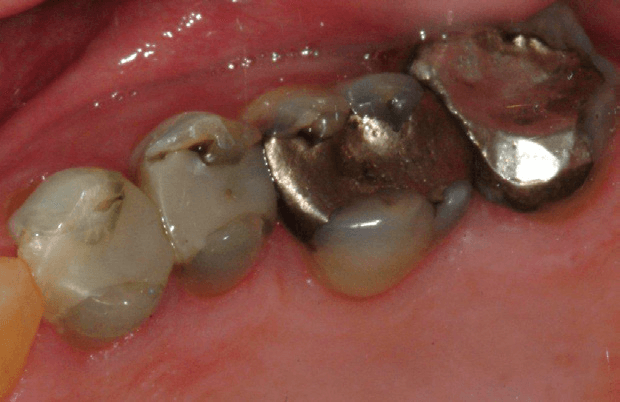
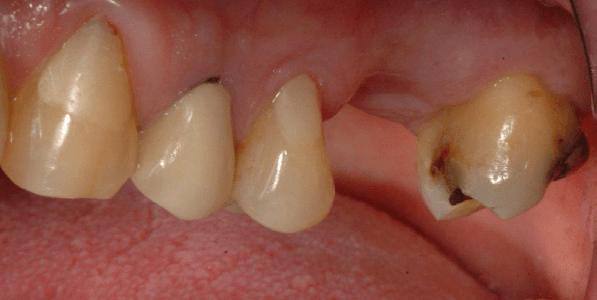
Tooth Coloured Filling

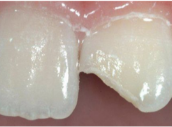
Cracked Filling

Worn Filling

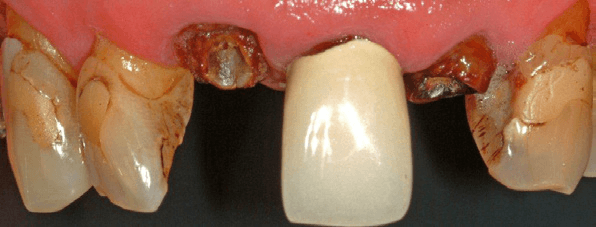
Foundation Filling Prior to Crown Placement
- An amalgam separator must be properly installed, utilized, and maintained to collect mercury amalgam waste so that it is not released into the effluent from the dental office.
- Each room where mercury fillings are removed must have adequate filtration in place, which requires a high-volume air filtration system (such as an at source oral aerosol vacuum) capable of removing mercury vapor and amalgam particles generated during the removal of one or more mercury fillings.
- If possible, windows should be opened to reduce the mercury concentration in the air.
- The patient will be given a slurry of charcoal, chlorella, or similar adsorbent to rinse and swallow before the procedure (unless the patient declines or there are other contraindications making this clinically inappropriate).
- Protective gowns and covers for the dentist, dental personnel, and the patient must be in place. All present in the room must be protected because substantial quantities of particles generated during the procedure will elude collection by suction devices. It has been demonstrated that these particles can be spread from the patient’s mouth to the hands, arms, face, chest and other parts of the dental worker’s and patient’s anatomy.
- Non-latex nitrile gloves must be utilized by the dentist and all dental personnel in the room.
- Face shields and hair/head coverings are to be utilized by the dentist and all dental personnel in the room.
- Either a properly-sealed, respiratory grade mask rated to capture mercury or a positive pressure, properly-sealed mask providing air or oxygen must be worn by the dentist and all dental personnel in the room.
- In order to protect the patient’s skin and clothing, a full body, impermeable barrier, as well as a full head/face/neck barrier under/around the dam, need to be utilized.
- External air or oxygen delivered via a nasal mask for the patient also needs to be utilized to assure the patient does not inhale any mercury vapor or amalgam particulate during the procedure. A nasal cannula is an acceptable alternative for this purpose as long as the patient’s nose is completely covered with an impermeable barrier.
- A dental dam that is made with non-latex nitrile material must be placed and properly sealed in the patient’s mouth.
- A saliva ejector must be placed under the dental dam to reduce mercury exposure to the patient.
- During amalgam filling removal, the dentist must utilize an at source oral aerosol vacuum in close proximity to the operating field (i.e., two to four inches from the patient’s mouth) to mitigate mercury exposure.
- High speed evacuation produces better capture when fitted with a Clean Up device, which is not mandatory but is preferred.
- Copious amounts of water to reduce heat and a conventional high speed evacuation device to capture mercury discharges are required to reduce ambient mercury levels.
- The amalgam needs to be sectioned into chunks and removed in as large of pieces as possible, using a small diameter carbide drill.
- Once the removal process is complete, the patient’s mouth should be thoroughly flushed with water and then rinsed out with a slurry of charcoal, chlorella or similar adsorbent.
- Dentists must comply with federal, state, and local regulations addressing the proper handling, cleaning, and/or disposal of mercury-contaminated components, clothing, equipment, surfaces of the room, and flooring in the dental office.
- During the opening and maintenance of suction traps in operatories or on the main suction unit, dental staff should utilize the appropriate personal protection equipment described above.
It is important to note that as a safety precaution, the IAOMT does not recommend amalgam filling removal for women who are pregnant or breast-feeding and that the IAOMT does not recommend that dental personnel who are pregnant or breast-feeding conduct work that disrupts amalgam fillings (including their removal).
All of this information as well as a complete list of references can be found at https://iaomt.org/resources/safe-removal-amalgam-fillings
Why might I request to have my Silver Fillings removed?
- Esthetics – The removal of a silver restoration to be replaced with a material that matches the color of the natural tooth.
- Health – To decrease potential exposure to the mercury vapor released from silver (amalgam) fillings. The safety and health risks of this vapor is widely debated. However, despite their wide use, overall use of silver fillings is declining worldwide
What is involved in having my Silver Fillings removed?
- The procedure may be simple or more complex depending on the choice of dental material selected to replace the silver filling.
- The removal of silver fillings can be done using a controlled office protocol to reduce exposure to mercury vapor and remove environmental risk.
What are the risks associated with having my Silver Fillings removed?
- You may experience temperature and bite sensitivity associated with the new restoration which can last for a few days or up to three months.
- Less commonly, a tooth may have irreversible irritation involving the need for root canal therapy and a subsequent crown.
- Pregnant women should avoid having silver (amalgam) fillings removed to avoid any negative effects on the fetus.
When might my dentist recommend my Silver Fillings be removed?
- When the silver filling no longer provides an adequate seal for the tooth, resulting in leakage and decay.
- When the silver filling needs to be removed and the tooth evaluated prior to crown placement.
- When the silver filling is cracked or worn.
What happens if I choose not to have my Silver Fillings removed?
- Esthetic concerns will not be addressed. However, the health of the tooth may not be compromised and may last many years if the silver filling is sealing the tooth and functioning properly.
- If removal of the silver filling has been recommended for decay, leakage or possible fracture, then these teeth will have continued or increasing risks, and repair options will become more complex over time.
- There will be ongoing potential for exposure to mercury vapor.

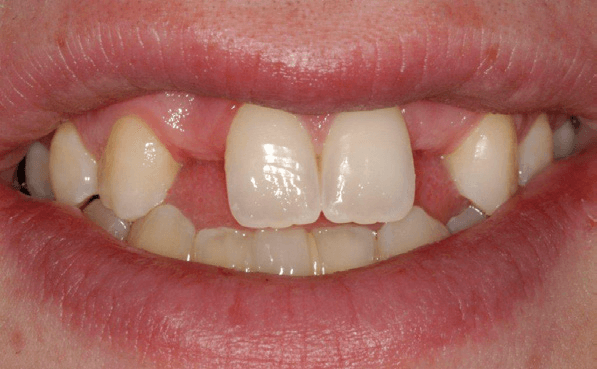
Tooth colored filling to repair chipped front tooth


Space closure with fillings


Silver filling replacement
What material is in a Tooth Colored Filling?
A tooth-colored filling is a mixture of a tooth-colored resin with clear glass particles that give it strength.
What are the benefits of a Tooth Colored Filling?
Tooth colored fillings come in many shades so they very closely match the color of natural teeth. They are bonded into place and require less removal of healthy tooth structure than silver fillings.
What are the risks of a Tooth Colored Filling?
As with any filling, having a tooth colored filling involves some inherent risks both to the remaining tooth structure and to the tooth colored filling itself:
- Tooth colored fillings are limited because they seal a tooth but do not prevent it from breaking
- Tooth colored fillings may fracture; the larger the tooth colored fillings, the greater the risk of fracture
- Tooth colored fillings may decay around the edge of the filling if your dentist is unable to keep the tooth clean and dry while placing the tooth colored filling
- Preparing for and placing a tooth colored filling can irritate the tooth and cause “post-operative” sensitivity which may last for up to 3 months
- Teeth which have had tooth colored fillings may need a root canal treatment less than 1% of the time during the lifetime of the tooth
What are the alternatives to having a Tooth Colored Filling?
The alternatives to having a tooth colored filling are:
- Having a silver filling or “amalgam” placed
- Having a gold or porcelain inlay/onlay restoration placed
How can an existing bite affect a Tooth Colored Filling?
Bite problems may lead to the tooth-colored filling or tooth breaking or loosening.
Are there any post-treatment restrictions once I have a Tooth Colored Filling?
- A tooth colored filling may have a good color match with your natural tooth when it is placed but less of a match as your natural tooth ages
- Tooth colored fillings can collect stain over time from foods such as black tea, coffee and wine
- Tooth colored fillings may chip or break if used for abnormal activities (e.g., biting fishing line, sewing thread or finger nails, opening bottles).


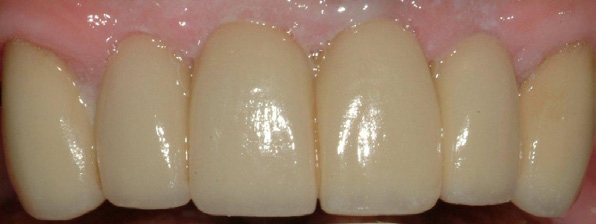
Porcelain crowns build back smile
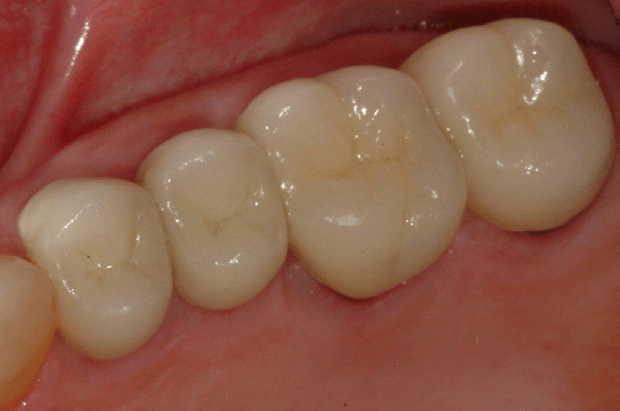
Porcelain fused to metal crowns build back natural tooth appearance and function
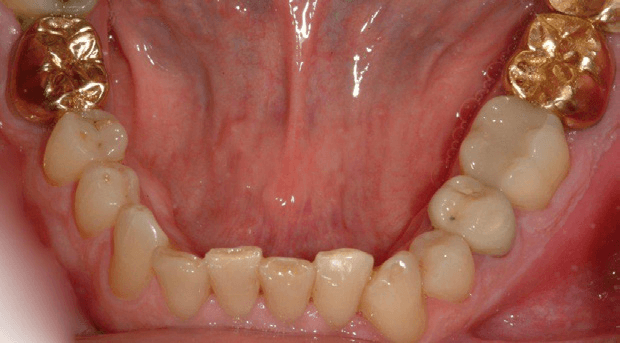
Gold crowns build back function
What materials are in a Tooth Supported Crown?
Crowns are made of three types of materials:
- Porcelain – most like a natural tooth in color
- Gold Alloy – strongest and most conservative in its preparation
- Porcelain fused to an inner core of gold alloy (Porcelain Fused to Metal or “PFM”) – combines strength and aesthetics
What are the benefits of having a Tooth Supported Crown?
Crowns restore a tooth to its natural size, shape and—if using porcelain—color. They improve the strength, function and appearance of a broken down tooth that may otherwise be lost. They may also be designed to decrease the risk of root decay.
What are the risks of having a Tooth Supported Crown?
In having a crown, some inherent risks exist both to the tooth and to the crown itself. The risks to the tooth are:
- Preparation for a crown weakens tooth structure and permanently alters the tooth underneath the crown
- Preparing for and placing a crown can irritate the tooth and cause “post-operative” sensitivity, which may last up to 3 months
- The tooth underneath the crown may need a root canal treatment about 6% of the time during the lifetime of the tooth
- If the cement seal at the edge of the crown is lost, decay may form at the juncture of the crown and tooth
The risks to the crown are:
- Porcelain may chip and metal may wear over time
- If the tooth needs a root canal treatment after the crown is permanently cemented, the procedure may fracture the crown and the crown may need to be replaced.
What are the alternatives to Tooth Supported Crowns?
Alternatives to crowns are fillings, such as composite or silver amalgam. These restorations remove decay and may restore teeth to their original form, but are limited because they do not improve the strength of broken down teeth. They also do not decrease the risk of root decay or improve the long term function and aesthetics of broken down teeth or crowns.
How can an existing bite affect a Tooth Supported Crown?
- Excessive bite forces may lead to the tooth under the crown breaking or loosening
- Excessive bite forces may lead to the crown chipping, breaking or loosening
Are there any post-treatment limitations once I have a Tooth Supported Crown?
- Porcelain on a crown may have a good color match with adjacent natural teeth when the crown is placed, but less of a match as your natural teeth age
- Gum recession may lead to unsightly dark roots or crown margins becoming visible
- A crown may chip or break if used for abnormal activities (e.g., biting fishing line, sewing thread or finger nails, opening bottles)
Fills spaces

Builds back smile
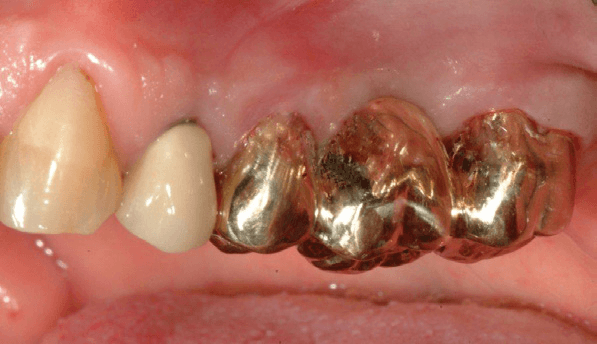
Restores function
What material is in a Tooth Supported Bridge?
Bridges are made of three types of materials:
- Porcelain – most like a natural tooth in color
- Gold Alloy – strongest and most conservative in its preparation
- Porcelain fused to an inner core of gold alloy (Porcelain Fused to Metal or “PFM”) – combines strength and aesthetics
What are the benefits of having a Tooth Supported Bridge?
Bridges build back your smile and help you to speak and chew properly by restoring your teeth to their natural size, shape, and— if using porcelain— color. They help maintain tooth, bite, and jaw alignment by preventing remaining teeth from shifting out of position.
What are the risks of having a Tooth Supported Bridge?
In having a bridge, some inherent risks exist both to the tooth and to the bridge itself. The risks to the remaining teeth are:
- Preparation for a bridge weakens tooth structure of the anchor teeth and permanently alters the teeth
- Preparing for and placing a bridge can irritate the anchor teeth and cause “post-operative” sensitivity which may last for up to 3 months
- Anchor teeth for bridges may need root canal treatment about 6% of the time during the lifetime of the tooth
- Anchor teeth may become mobile if there is bone loss around their roots • If the cement seal at the edge of the crown over an anchor tooth is lost, decay may form at the juncture of the crown and tooth
The risks to the bridge are:
- Porcelain may chip and metal may wear over time
- If a tooth needs a root canal treatment after the bridge is permanently cemented, the procedure may fracture the bridge and the bridge may need to be replaced
- The longer the bridge, the shorter the lifespan; three tooth bridges last 10-15 years on average
What are the alternatives to having a Tooth Supported Bridge?
Three alternatives to bridges exist:
- Replace the missing tooth with an implant
- Replace the missing tooth with a removable partial denture
- Leave the space as is
How can an existing bite affect a Tooth Supported Bridge?
- Excessive biting forces or untreated bite problems may lead to the anchor teeth breaking or loosening
- Excessive biting forces or untreated bite problems may lead to the bridge chipping, breaking or loosening
Are there any post-treatment limitations once I have a Tooth Supported Bridge?
• As a bridge is made in one solid piece, it is not possible to floss in
between the teeth; special dental aids must be used to maintain
the health of the anchor teeth and gums around the bridge
• Porcelain on the bridge may have a good color match with adjacent natural
teeth when the bridge is placed but less of a match as your natural teeth age
• Food may become lodged under fixed bridges; gum recession over time may
make food impaction unavoidable, even with the most ideal bridge contour
• Gum recession may lead to unsightly dark roots or bridge margins
becoming visible
• A bridge may chip or break if used for abnormal activities (e.g., biting
fishing line, sewing thread or finger nails, opening bottles)
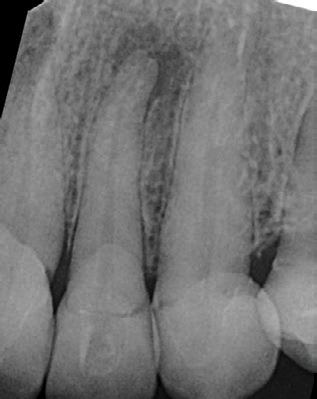
Before Root Canal
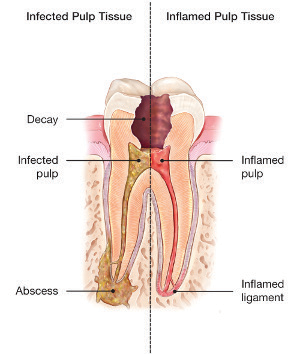

After Root Canal
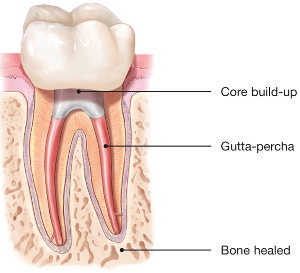
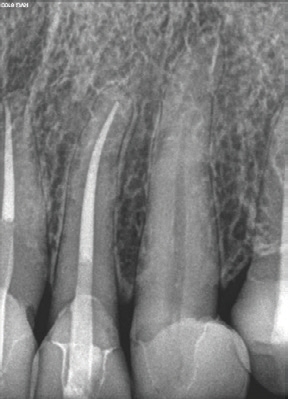
After Root Canal
What would cause the nerve of a tooth to die or become infected?
- The nerve of a tooth can be damaged if a tooth is cracked or fractured. Deep decay or trauma, like a blow to the tooth or from a fall may also cause damage.
- Even when carefully performed, every fi lling and crown has an impact on the tooth’s nerve health, so teeth with large fi llings or crowns are more likely to need a root canal.
What are the benefits of having root canal treatment?
- A tooth can be saved that would otherwise have to be removed due to infection or nerve damage.
- Chronic infl ammation that occurs with infection may be eliminated. This infl ammation is harmful to your overall health and the infection can spread to other parts of the body, including your brain and heart, and can be fatal.
- Pain or sensitivity caused by the damaged nerve can be relieved.
Are there risks associated with root canal treatment?
- Although 90% of root canal treatments are successful, a small number will require a second root canal procedure or additional treatment on the root tip.
- Even with the best care, root canal treatment may not resolve all the infection or infl ammation. In those cases, the tooth may still be lost, usually due to a hidden deep crack in the tooth or a root canal system too small to be adequately cleaned and sealed.
Will further treatment be needed following root canal treatment?
- On a back tooth, a crown is needed to lower the risk of future cracking or fracture from chewing forces. If the tooth already has a healthy, well-sealed crown, the dentist may be able to seal the root canal without replacing the crown.
- A front tooth in good condition may only need a bonded filling to seal and support it. Your dentist will discuss what support your specific tooth will need.
Are there any alternatives to undergoing root canal treatment?
The only alternative would be to remove the tooth.
Patient Feedback
EXCELLENTTrustindex verifies that the original source of the review is Google. Great staff and care at Bend Dental Wellness!Trustindex verifies that the original source of the review is Google. We have been going here for 5 years. We really enjoy how kind all of the staff are. Up to date modern tools.Trustindex verifies that the original source of the review is Google. I had an emergency and they found a way to get me in to be seen the same day. The staff and Dr Quigley were helpful and professional. I’ve been going to Bend Dental Wellness for four years and it has always been professional and friendly.Trustindex verifies that the original source of the review is Google. Dr. Blake Q and his staff are very friendly and competent. I did choose this practice because of his 'better' practices with dental care. And I've been very satisfied with my dental care for the past 3+years and will continue. Had a cleaning today with Mara and she was very gentle and thorough.Trustindex verifies that the original source of the review is Google. The service was excellent, both my teeth cleaning and discussion of possible future needs.
Request An Appointment
Need help? Contact us!